Neurodevelopmental disorder
Neurodevelopmental disorder
Jump to navigation
Jump to search
This article with questionable factual accuracy needs more medical references for verification or relies too heavily on primary sources. (November 2014) |
| Neurodevelopmental disorder | |
|---|---|
| Specialty | Psychiatry |
Neurodevelopmental disorder is a mental disorder. A narrower use of the term refers to a disorder of brain function which affects emotion, learning ability, self-control and memory and which unfolds as the individual grows. Neurodevelopmental disorders tend to last for a persons entire lifetime.
Contents
1 Types
2 Causes
2.1 Deprivation
2.2 Genetic disorders
2.3 Immune dysfunction
2.4 Infectious diseases
2.5 Metabolic disorders
2.6 Nutrition
2.7 Physical trauma
3 Diagnosis
3.1 Definition
4 Consequences
5 See also
6 Bibliography
7 Notes
8 External links
Types[edit]
Disorders considered neurodevelopmental in origin include:
Intellectual disability (ID) or intellectual and developmental disability (IDD), previously called mental retardation
Autism spectrum disorders, such as Asperger's syndrome or Kanner syndrome
Motor disorders including developmental coordination disorder and stereotypic movement disorder
Tic disorders including Tourette's syndrome
Traumatic brain injury (including congenital injuries such as those that cause cerebral palsy[1])- Communication, speech and language disorders
- Genetic disorders, such as fragile-X syndrome, Down syndrome,[2]attention deficit hyperactivity disorder, schizophrenia, schizotypal disorder, hypogonadotropic hypogonadal syndromes[3]
- Disorders due to neurotoxicants like fetal alcohol spectrum disorder, Minamata disease caused by mercury, behavioral disorders including conduct disorder etc. caused by other heavy metals, such as lead, chromium, platinum etc., hydrocarbons like dioxin, PBDEs and PCBs, medications and illegal drugs, like cocaine and others.
Causes[edit]
The development of the nervous system including the brain is orchestrated, tightly regulated, and genetically encoded process with clear influence from the environment. This suggests that any deviation from this program early in life can result in neurodevelopmental disorders and, depending on specific timing, might lead to distinct pathology later in life.[4] Because of that, there are many causes of neurodevelopmental disorder, which can range from deprivation, genetic and metabolic diseases, immune disorders, infectious diseases, nutritional factors, physical trauma, and toxic and environmental factors.
Some neurodevelopmental disorders—such as autism and other pervasive developmental disorders—are considered multifactorial syndromes with many causes but more specific neurodevelopmental manifestation.[5]
Deprivation[edit]
Deprivation from social and emotional care causes severe delays in brain and cognitive development. Studies with children growing up Romanian orphanages during Nicolae Ceauşescu's regime reveal profound effects of social deprivation and language deprivation on the developing brain. These effects are time dependent. The longer children stayed in negligent institutional care, the greater the consequences. By contrast, adoption at an early age mitigated some of the effects of earlier institutionalization (abnormal psychology).[6]
Genetic disorders[edit]

A child with Down syndrome
A prominent example of a genetically determined neurodevelopmental disorder is Trisomy 21, also known as Down syndrome. This disorder usually results from an extra chromosome 21, although in uncommon instances it is related to other chromosomal abnormalities such as translocation of the genetic material. It is characterized by short stature, epicanthal (eyelid) folds, abnormal fingerprints, and palm prints, heart defects, poor muscle tone (delay of neurological development) and mental retardation (delay of intellectual development).[2]
Less commonly known genetically determined neurodevelopmental disorders include Fragile X syndrome. Fragile X syndrome was first described in 1943 by J.P. Martin and J. Bell, studying persons with family history of sex-linked "mental defects".[7]Rett syndrome, another X-linked disorder, produces severe functional limitations.[8]Williams syndrome is caused by small deletions of genetic material from chromosome 7.[9]
The most common recurrent Copy Number Variannt disorder is 22q11.2 deletion syndrome (formerly DiGeorge or velocardiofacial syndrome), followed by Prader-Willi syndrome and Angelman syndrome.[10]
Immune dysfunction[edit]
Immune reactions during pregnancy, both maternal and of the developing child, may produce neurodevelopmental disorders. One typical immune reaction in infants and children is PANDAS,[11] or Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal infection.[12] Another disorder is Sydenham's chorea, which results in more abnormal movements of the body and fewer psychological sequellae. Both are immune reactions against brain tissue that follow infection by Streptococcus bacteria. Susceptibility to these immune diseases may be genetically determined,[13] so sometimes several family members may suffer from one or both of them following an epidemic of Strep infection.
Infectious diseases[edit]
Systemic infections can result in neurodevelopmental consequences, when they occur in infancy and childhood of humans, but would not be called a primary neurodevelopmental disorder per se, as for example HIV[14] Infections of the head and brain, like brain abscesses, meningitis or encephalitis have a high risk of causing neurodevelopmental problems and eventually a disorder. For example, measles can progress to subacute sclerosing panencephalitis.
A number of infectious diseases can be transmitted either congenitally (before or at birth), and can cause serious neurodevelopmental problems, as for example the viruses HSV, CMV, rubella (congenital rubella syndrome), Zika virus, or bacteria like Treponema pallidum in congenital syphilis, which may progress to neurosyphilis if it remains untreated. Protozoa like Plasmodium[14] or Toxoplasma which can cause congenital toxoplasmosis with multiple cysts in the brain and other organs, leading to a variety of neurological deficits.
Some cases of schizophrenia may be related to congenital infections though the majority are of unknown causes.[15]
Metabolic disorders[edit]
Metabolic disorders in either the mother or the child can cause neurodevelopmental disorders. Two examples are diabetes mellitus (a multifactorial disorder) and phenylketonuria (an inborn error of metabolism). Many such inherited diseases may directly affect the child's metabolism and neural development[16] but less commonly they can indirectly affect the child during gestation. (See also teratology).
In a child, type 1 diabetes can produce neurodevelopmental damage by the effects of excess or insufficient glucose. The problems continue and may worsen throughout childhood if the diabetes is not well controlled.[17]Type 2 diabetes may be preceded in its onset by impaired cognitive functioning.[18]
A non-diabetic fetus can also be subjected to glucose effects if its mother has undetected gestational diabetes. Maternal diabetes causes excessive birth size, making it harder for the infant to pass through the birth canal without injury or it can directly produce early neurodevelopmental deficits. Usually the neurodevelopmental symptoms will decrease in later childhood.[19]
Phenylketonuria, also known as PKU, can induce neurodevelopmental problems and children with PKU require a strict diet to prevent mental retardation and other disorders. In the maternal form of PKU, excessive maternal phenylalanine can be absorbed by the fetus even if the fetus has not inherited the disease. This can produce mental retardation and other disorders.[20][21]
Nutrition[edit]
Nutrition disorders and nutritional deficits may cause neurodevelopmental disorders, such as spina bifida, and the rarely occurring anencephaly, both of which are neural tube defects with malformation and dysfunction of the nervous system and its supporting structures, leading to serious physical disability and emotional sequelae. The most common nutritional cause of neural tube defects is folic acid deficiency in the mother, a B vitamin usually found in fruits, vegetables, whole grains, and milk products.[22][23] (Neural tube defects are also caused by medications and other environmental causes, many of which interfere with folate metabolism, thus they are considered to have multifactorial causes.)[24][25] Another deficiency, iodine deficiency, produces a spectrum of neurodevelopmental disorders ranging from mild emotional disturbance to severe mental retardation. (see also cretinism)
Excesses in both maternal and infant diets may cause disorders as well, with foods or food supplements proving toxic in large amounts. For instance in 1973 K.L. Jones and D.W. Smith of the University of Washington Medical School in Seattle found a pattern of "craniofacial, limb, and cardiovascular defects associated with prenatal onset growth deficiency and developmental delay" in children of alcoholic mothers, now called fetal alcohol syndrome, It has significant symptom overlap with several other entirely unrelated neurodevelopmental disorders.[26] It has been discovered that iron supplementation in baby formula can be linked to lowered I.Q. and other neurodevelopmental delays.[27]
Physical trauma[edit]
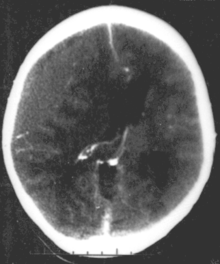
CT scan showing epidural hematoma, a type of traumatic brain injury (upper left)
Brain trauma in the developing human is a common cause (over 400,000 injuries per year in the US alone, without clear information as to how many produce developmental sequellae)[28] of neurodevelopmental syndromes. It may be subdivided into two major categories, congenital injury (including injury resulting from otherwise uncomplicated premature birth)[1] and injury occurring in infancy or childhood. Common causes of congenital injury are asphyxia (obstruction of the trachea), hypoxia (lack of oxygen to the brain) and the mechanical trauma of the birth process itself.
Diagnosis[edit]
Traditionally, genetic abnormalities in neurodevelopmental disorders were detected using karyotype analysis, which found 5% of relevant disorders. As of 2017[update], chromosomal microarray analysis (CMA) has replaced karyotyping, because of its greater diagnostic yield in about 20% of cases, detecting smaller chromosome abnormalities. It is the first line genomic test.[10]
New descriptions include the term Copy-number variants (CNVs), which are losses or gains of chromosomal regions greater than 1 kb in length.[10] CNVs are mentioned with the chromosomal band(s) they involve and their genome sequence coordinates. CNVs can be nonrecurrent and recurrent.[10]
With CMA costs of testing have increased from $800 US to $1500. Guidelines from the American College of Medical Genetics and Genomics and the American Academy of Pediatrics recommend CMA as standard of care in the US.[10]
Definition[edit]
Neurodevelopmental disorders[29] are impairments of the growth and development of the brain or central nervous system. A narrower use of the term refers to a disorder of brain function that affects emotion, learning ability, self-control and memory and that unfolds as an individual develops and grows.
The term is sometimes erroneously used as an exclusive synonym for autism spectrum disorders.[citation needed]
Consequences[edit]
Neurodevelopmental disorders are in their multitude associated with widely varying degrees of difficulty, depending on which there are different degrees of mental, emotional, physical, and economic consequences for individuals, and in turn families, groups and society.
See also[edit]
- Epigenetics
- Microcephaly
- Reverse learning
- Teratology
Bibliography[edit]
Tager-Flusberg, Helen (1999). Neurodevelopmental disorders. Cambridge, Massachusetts: MIT Press. ISBN 978-0-262-20116-2..mw-parser-output cite.citationfont-style:inherit.mw-parser-output qquotes:"""""""'""'".mw-parser-output code.cs1-codecolor:inherit;background:inherit;border:inherit;padding:inherit.mw-parser-output .cs1-lock-free abackground:url("//upload.wikimedia.org/wikipedia/commons/thumb/6/65/Lock-green.svg/9px-Lock-green.svg.png")no-repeat;background-position:right .1em center.mw-parser-output .cs1-lock-limited a,.mw-parser-output .cs1-lock-registration abackground:url("//upload.wikimedia.org/wikipedia/commons/thumb/d/d6/Lock-gray-alt-2.svg/9px-Lock-gray-alt-2.svg.png")no-repeat;background-position:right .1em center.mw-parser-output .cs1-lock-subscription abackground:url("//upload.wikimedia.org/wikipedia/commons/thumb/a/aa/Lock-red-alt-2.svg/9px-Lock-red-alt-2.svg.png")no-repeat;background-position:right .1em center.mw-parser-output .cs1-subscription,.mw-parser-output .cs1-registrationcolor:#555.mw-parser-output .cs1-subscription span,.mw-parser-output .cs1-registration spanborder-bottom:1px dotted;cursor:help.mw-parser-output .cs1-hidden-errordisplay:none;font-size:100%.mw-parser-output .cs1-visible-errorfont-size:100%.mw-parser-output .cs1-subscription,.mw-parser-output .cs1-registration,.mw-parser-output .cs1-formatfont-size:95%.mw-parser-output .cs1-kern-left,.mw-parser-output .cs1-kern-wl-leftpadding-left:0.2em.mw-parser-output .cs1-kern-right,.mw-parser-output .cs1-kern-wl-rightpadding-right:0.2em
Brooks, David R.; Walter Wolfgang Fleischhacker (2006). Neurodevelopmental Disorders. Berlin: Springer. ISBN 978-3-211-26291-7.
Notes[edit]
^ ab Murray RM, Lewis SW (September 1987). "Is schizophrenia a neurodevelopmental disorder?". Br Med J (Clin Res Ed). 295 (6600): 681–2. doi:10.1136/bmj.295.6600.681. PMC 1247717. PMID 3117295.
^ ab Facts about down syndrome Archived 2012-04-03 at the Wayback Machine.
^ Hernan Valdes-Socin, Matilde Rubio Almanza, Mariana Tomé Fernández-Ladreda, et al. Reproduction, smell, and neurodevelopmental disorders: genetic defects in different hypogonadotropic hypogonadal syndromes. Frontiers in Endocrinology 2014, 5: 109. review
^
Pletikos, Mihovil; Sousa, Andre MM; et al. (22 January 2014). "Temporal Specification and Bilaterality of Human Neocortical Topographic Gene Expression". Neuron. 81 (2): 321–332. doi:10.1016/j.neuron.2013.11.018. PMC 3931000. PMID 24373884.
^ Samaco RC, Hogart A, LaSalle JM (February 2005). "Epigenetic overlap in autism-spectrum neurodevelopmental disorders: MECP2 deficiency causes reduced expression of UBE3A and GABRB3". Hum. Mol. Genet. 14 (4): 483–92. doi:10.1093/hmg/ddi045. PMC 1224722. PMID 15615769.
^ Nelson C.A.; et al. (2007). "Cognitive Recovery in Socially Deprived Young Children: The Bucharest Early Intervention Project". Science.
^ Martin JP, Bell J (1943). "A pedigree of mental defect showing sex-linkage". J. Neurol. Psychiat. 6 (3–4): 154–7. doi:10.1136/jnnp.6.3-4.154. PMC 1090429. PMID 21611430.
^ Amir RE, Van den Veyver IB, Wan M, Tran CQ, Francke U, Zoghbi HY (October 1999). "Rett syndrome is caused by mutations in X-linked MECP2, encoding methyl-CpG-binding protein 2". Nat. Genet. 23 (2): 185–8. doi:10.1038/13810. PMID 10508514.
^ Merla G, Howald C, Henrichsen CN, et al. (August 2006). "Submicroscopic Deletion in Patients with Williams-Beuren Syndrome Influences Expression Levels of the Nonhemizygous Flanking Genes". Am. J. Hum. Genet. 79 (2): 332–41. doi:10.1086/506371. PMC 1559497. PMID 16826523.
^ abcde Christa Lese Martin, David H. Ledbetter. Chromosomal Microarray Testing for Children With Unexplained Neurodevelopmental Disorders JAMA. 2017;317(24):2545–2546. doi:10.1001/jama.2017.7272 June 27, 2017
^ Pavone, P.; et al. (2004). "Anti-brain antibodies in PANDAS versus uncomplicated streptococcal infection". Pediatr Neurol. 30 (2): 107–110. doi:10.1016/S0887-8994(03)00413-2. hdl:2108/194065. PMID 14984902.
^ Dale, RC.; et al. (2005). "Incidence of anti-brain antibodies in children with obsessive–compulsive disorder". Br J Psychiatry. 187 (4): 314–319. doi:10.1192/bjp.187.4.314. PMID 16199788. Retrieved 2008-08-17.
^ Swedo, Susan E (December 2001). "Genetics of childhood disorders: XXXIII autoimmunity part 6: poststreptoccoal autoimmunity". Reprinted from J Am Acad Child Adolesc Psychiatry, 40:12,1479-1482. Retrieved 2008-08-17.
^ ab Bolvin, MJ; Kakooza, AM; Warf, BC; Davidson, LL; Grigorenko, EL (November 2015). "Reducing neurodevelopmental disorders and disability through research and interventions". Nature. 527 (7578): S155–60. doi:10.1038/nature16029. PMID 26580321.
^ "Prenatal infection as a risk factor for schizophrenia – Brown 32 (2): 200 – Schizophrenia Bulletin". Retrieved 2008-08-10.
^ Richardson, A.J.; Ross, M.A. (July 2000). "Fatty acid metabolism in neurodevelopmental disorder: a new perspective on associations between attention-deficit/hyperactivity disorder, dyslexia, dyspraxia, and the autistic spectrum". Prostaglandins, Leukotrienes and Essential Fatty Acids. 63 (1–2): 1–9. doi:10.1054/plef.2000.0184. PMID 10970706.
^ Nordham, Elizabeth A; Anderson, PJ; Jacobs, R; Hughes, M; Warne, GL; Werther, GA; et al. (2001). "Neuropsychological Profiles of Children With Type 1 Diabetes 6 Years After Disease Onset". Diabetes Care. 24 (9): 1541–1546. doi:10.2337/diacare.24.9.1541. PMID 11522696.
^ Olsson, Gunilla M.; Hulting, AL; Montgomery, SM; et al. (2008). "Cognitive Function in Children and Subsequent Type 2 Diabetes: Response to Batty, Gale, and Deary". Diabetes Care. 31 (3): 514–516. doi:10.2337/dc07-1399. PMC 2453642. PMID 18083794.
^ Ornoy A, Wolf A, Ratzon N, Greenbaum C, Dulitzky M (July 1999). "Neurodevelopmental outcome at early school age of children born to mothers with gestational diabetes". Arch. Dis. Child. Fetal Neonatal Ed. 81 (1): F10–4. PMC 1720965. PMID 10375355.
^ Lee PJ, Ridout D, Walter JH, Cockburn F (February 2005). "Maternal phenylketonuria: report from the United Kingdom Registry 1978-97". Arch. Dis. Child. 90 (2): 143–6. doi:10.1136/adc.2003.037762. PMC 1720245. PMID 15665165.
^ Rouse B, Azen C, Koch R, et al. (March 1997). "Maternal Phenylketonuria Collaborative Study (MPKUCS) offspring: facial anomalies, malformations, and early neurological sequelae". Am. J. Med. Genet. 69 (1): 89–95. doi:10.1002/(SICI)1096-8628(19970303)69:1<89::AID-AJMG17>3.0.CO;2-K. PMID 9066890.
^ "Folic Acid - March of Dimes".
^ "Folate (Folacin, Folic Acid)".
^ "Folic scid: topic home". Centers for Disease Control and Prevention. U.S. Department of Health and Human Services. Retrieved 2008-08-02.
^ "The basics about spina bifida". Centers for Disease Control and Prevention. U.S. Department of Health and Human Services. Retrieved 2008-08-02.
^ Fetal alcohol syndrome: guidelines for referral and diagnosis (PDF). CDC (July 2004). Retrieved on 2007-04-11
^ Kerr, Martha; Désirée Lie (2008). "Neurodevelopmental delays associated with iron-fortified formula for healthy infants". Medscape Psychiatry and Mental Health. Retrieved 2008-08-04.
^ "Facts About TBI" (PDF). Retrieved 2008-08-06.
^ Reynolds, Cecil R.; Goldstein, Sam (1999). Handbook of neurodevelopmental and genetic disorders in children. New York: The Guilford Press. pp. 3–8. ISBN 978-1-57230-448-2.
External links[edit]
Neurodevelopmental Disorders at Curlie
A Review of Neurodevelopmental Disorders - Medscape review
Categories:
- Childhood psychiatric disorders
- Developmental neuroscience
- Neurological disorders
- Neurodevelopmental disorders
(window.RLQ=window.RLQ||).push(function()mw.config.set("wgPageParseReport":"limitreport":"cputime":"0.568","walltime":"0.704","ppvisitednodes":"value":2341,"limit":1000000,"ppgeneratednodes":"value":0,"limit":1500000,"postexpandincludesize":"value":83697,"limit":2097152,"templateargumentsize":"value":1792,"limit":2097152,"expansiondepth":"value":12,"limit":40,"expensivefunctioncount":"value":6,"limit":500,"unstrip-depth":"value":1,"limit":20,"unstrip-size":"value":81328,"limit":5000000,"entityaccesscount":"value":4,"limit":400,"timingprofile":["100.00% 576.216 1 -total"," 35.38% 203.893 1 Template:Reflist"," 21.42% 123.444 16 Template:Cite_journal"," 18.75% 108.018 1 Template:Infobox_medical_condition_(new)"," 15.51% 89.344 1 Template:Infobox"," 13.71% 79.023 3 Template:Cite_book"," 11.58% 66.721 1 Template:MEDREF"," 7.26% 41.858 1 Template:Ambox"," 4.84% 27.871 1 Template:Citation_needed"," 4.54% 26.162 7 Template:Cite_web"],"scribunto":"limitreport-timeusage":"value":"0.307","limit":"10.000","limitreport-memusage":"value":8609113,"limit":52428800,"cachereport":"origin":"mw1328","timestamp":"20181231152408","ttl":1900800,"transientcontent":false);mw.config.set("wgBackendResponseTime":808,"wgHostname":"mw1328"););


